After every surgery, you will take the patient from the OR
and transport them to either the Post Anesthesia Care Unit (PACU) or the
Intensive Care Unit (ICU). Generally, patients only go to the ICU if they were
originally transported directly to the OR from either the ICU or Emergency
Department. Once you arrive, you will be transferring the care of the patient over
to the staff of each unit. In order to do so safely, you will need to learn how
to give a proper post-op report. In most instances this will be to a member of
the nursing staff, a resident in charge of patient care, or both. Everyone has
a different way they like to give their reports, but for the most part, it will
always include the same components. Below I have listed the things I consider
to be important. They are listed in the way that I present them to the staff
members, however you do not need to follow this same order. I do, however,
think it is helpful to give the report in the same way each time. It makes
things easier if you can find a rhythm.
In the PACU
- Patient name, age, and gender. (These may not always be obvious)
- Any known allergies along with a description of the associated reaction.
- What surgery the patient just underwent, including the surgical site. Pay attention to everything the surgeon did. If you are unsure, don’t be afraid to ask the nurse or a member of the surgical team before heading to the PACU.
- At this point you can also explain why the patient was having this procedure done in the first place, even if it seems obvious.
- Other significant medical conditions & history.
- This part can be tricky at times because you want to be thorough but are also on a bit of a time crunch. Use your best judgment to include things that may impact post-operative patient care. ie. HTN, cardiac issues, respiratory issues, neurological problems/deficits, renal/liver issues, sites of chronic pain, etc.
- It can be helpful to look at your pre-op interview sheet while talking to the nurse. Use it as a cheat sheet.
- This would be a good time to let them know about any preoperative lab values that may relate to their conditions (H/H, Blood glucose, Creatinine, etc.)
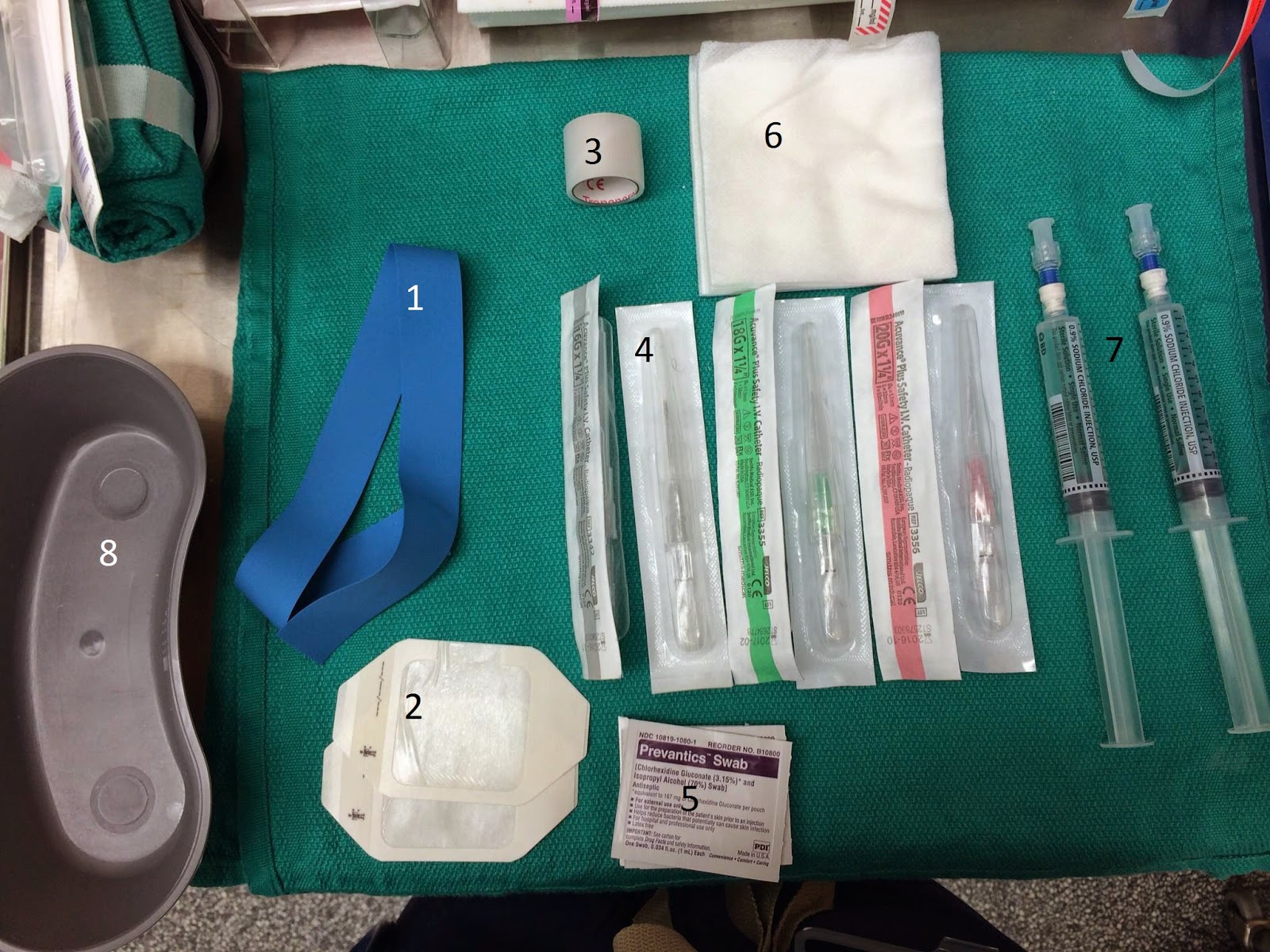
- Access sites – Be sure to include any peripheral IV’s, central lines, arterial lines, etc. Note if any of the lines have been giving you issues during the intraoperative period (Do they flush well? Are they positional? How is the CVP or arterial waveform?)
- Medications and totals given- They don’t need to know about every single medication. For example, they don’t necessarily need to know that you gave propofol and lidocaine at induction since this likely will not impact how they care for this patient. I have listed below the medications that I like to include.
- Premedication – Versed, Pepcid, Reglan, Albuterol, etc.These are particularly import for shorter procedures where the medication may still be active by the time the patient wakes up.
- Pain medications – Narcotics (fentanyl, morphine, dilaudid), NSAID (Torodol), Ofirmev, etc. Include general times of when you gave these. It can give the nurse a better idea of when they may need more.
- Anti-emetics – Decadron, Zofran, did you run the case as a TIVA?
- Antibiotics – Ancef, Vancomycin, Zosyn, Clindamycin, etc.Include the times given. The patient may need a redose soon.
- Beta blockers, anti-hypertensives, cardiac drugs- Metoprolol, Labetalol, Hydralazine, etc. Many of these medications have long half-lives that can last well in to the post-operative period and can have profound effects on hemodynamic stability.
- Paralytic and reversal – I don’t usually give totals of these medications, just let them know that they were given.
- Ins and Outs –
- Total fluid given – Distinguish amongst crystalloids, colloids, and blood products.
- Urine output
- Estimated blood loss
- Intraoperative course – How did the patient do during the procedure on our end of things.
- If the patient was stable the entire time, let them know that.
- BP issues- Hyper/hypotensive?
- EKG changes/changes in HR
- Respiratory troubles – problems oxygenating/ventilating?
- Difficulty managing the airway?
- Difficulty waking patient up?
- Any important lab value changes from ABG’s or VBG’s.
In the ICU
A report given in the ICU will be similar to one given in
PACU with a few minor differences:
- These staff are already familiar with these patients because they generally have been taking care of them for a period of time. For this reason, you do not need to include the patient’s medical history in your report.
- These patients are usually in pretty bad shape, that’s why they are in the ICU. They may already have a number of lines in. Just let the staff know if you added any new lines or took any out.
- Often times, you may take these patients to the ICU on drips in an effort to control hemodynamic stability or keep the patient sedated. Be sure to tell the staff of any infusions they are still on, at what rate they are going, and if you anticipate that they will need to stay on them.
- It is important to be very thorough in describing any intraoperative events. These can carry over into the ICU and may impact how the patient is managed.
- Patients will likely still be intubated. Specify if you would like any of the vent settings a specific way.
- All of the other components are the same as in your PACU report.
This may seem like a ton of information, but with some
practice, you can really make a report quick and concise while still including
all of the necessary information. Pay attention to how your instructors deliver
their reports and try to mimic their style while creating your own.